While the physiotherapy profession continues to grapple with how to address an entrenched split between mind and body in health care, we are facing an even larger challenge: a disconnect from the natural world. The concept of integrative health as applied to physiotherapy aims to improve upon how we address complexity and the intersection of body, mind, and environment (BME) (1). Such an approach promotes an integral approach that navigates health care in a way that frames and supports each person’s individual experience as representing a complex whole that is in inseparable relation to the environments that we live, work, and play in. With climate change advancing to the point of being a major public health issue, physiotherapists must come together to create new and improved pathways of meeting a broad spectrum of interacting needs at the individual, social/relational, community, and global levels.
Environment is best defined as a layered construct. It is helpful to consider that each person’s “mind-body” is “bathed” in (embedded into) various layers of environment such as the natural, built, organizational, social, cultural, economic, etc. We must carefully examine interactions and influences within the whole of each person’s, community’s, and/or culture’s past and present environment – and impact upon individual and public health. Is it more or less significant than we are giving attention to? How do we move away from only assessing and supporting this paradigm from an individual’s perspective and needs and consider the health of whole communities and populations? These are critical questions that we must explore together.
Movements such as the Environmental Physiotherapy Association (2, 3), the International Organization for Physiotherapy in Psychiatry and Mental Health (4), the Critical Physiotherapy Network (5), and the overall advancement of integrative and public health models within physiotherapy, carry intersectional potential to advance a larger agenda that the profession can play in global and planetary health.

Matt Erb
Physiotherapist, Associate Clinical Director, Faculty, Independent Scholar
Matt Erb is a physiotherapist in Tucson, Arizona. Matt has served as Associate Clinical Director for The Center for Mind-Body Medicine, is Founder of Embody Your Mind, and regularly teaches for the University of Arizona physician training programs.

My Experience
As a physiotherapist with over 25 years of experience, my clinical focus has been on mind-body integrated care for persistent health challenges (both somatic and mental, noting the semantic categorization that splits the two). It has been suggested that the growing chronic pain epidemic is a spokesmodel for biopsychosocial, integrative, or even just improved biomedical care that is whole-person oriented. True. And, I’ve come to the impression that we are falling short in the pervasive “body as machine” ontology as described by David Nicholls (6). While my journey through the academic, philosophical, and clinical world of mind-body medicine is ongoing, with no discernible destination, I’ve come to believe that professionalization (“physical”, “occupational”, etc.) is necessary and has also inadvertently caused harm in splitting off many elements that inform the whole-person experience of the ill health ← → well-being spectrum. Around 15 years ago a PT colleague and I were introduced to the public health focused work of The Center for Mind-Body (CMBM), whose aim is population-wide stress and trauma relief programming. Research into the model is demonstrating usefulness in a wide range of settings and cultures for challenges such as trauma (PTSD), anxiety, depression, worker burnout, war, violence, disaster relief, and more (7).
Built upon wisdom traditions and practices, and merged with scientific inquiry, the approach advocates for group-based experiences that are prosocial and collaborative, while still supporting individual phenomenological processes. Over my years of involvement with this work, I believe I’m coming to better recognize and understand hidden determinants that inform human experience and behavior. While the model does not meet all needs (none do), it has been a powerful forum out of which I have witnessed significant expressions and experiences of healing and transformation of longstanding, problematic content from people’s lives. I suggest that individual healing and inner work, what I prefer to call for myself the “psychospiritual domain” carries ripple effects that impact immediate interpersonal relationships, workspaces, communities, and our environment.
CMBM has long-standing community-based programs in war-impacted regions (e.g. Gaza, Israel, Kosovo, Ukraine); in schools impacted by mass gun violence (e.g. Broward Florida and Uvalde Texas); and in relation to climate change and climate disasters (e.g. cities and counties in Northern California following devastating wildfires; Houston, New Orleans, and Puerto Rico following hurricanes; Haiti following earthquakes). For the latter, I have joined a grassroots movement to assist in community preparedness. Many climate scientists say it is “when not if” that further climate-associated disasters will land. Recent research demonstrates that psychological distance (PD) as a barrier to climate action is lower than presumed and that it is not clear that reducing PD will reliably increase climate action (8). From this, we must ask what will?
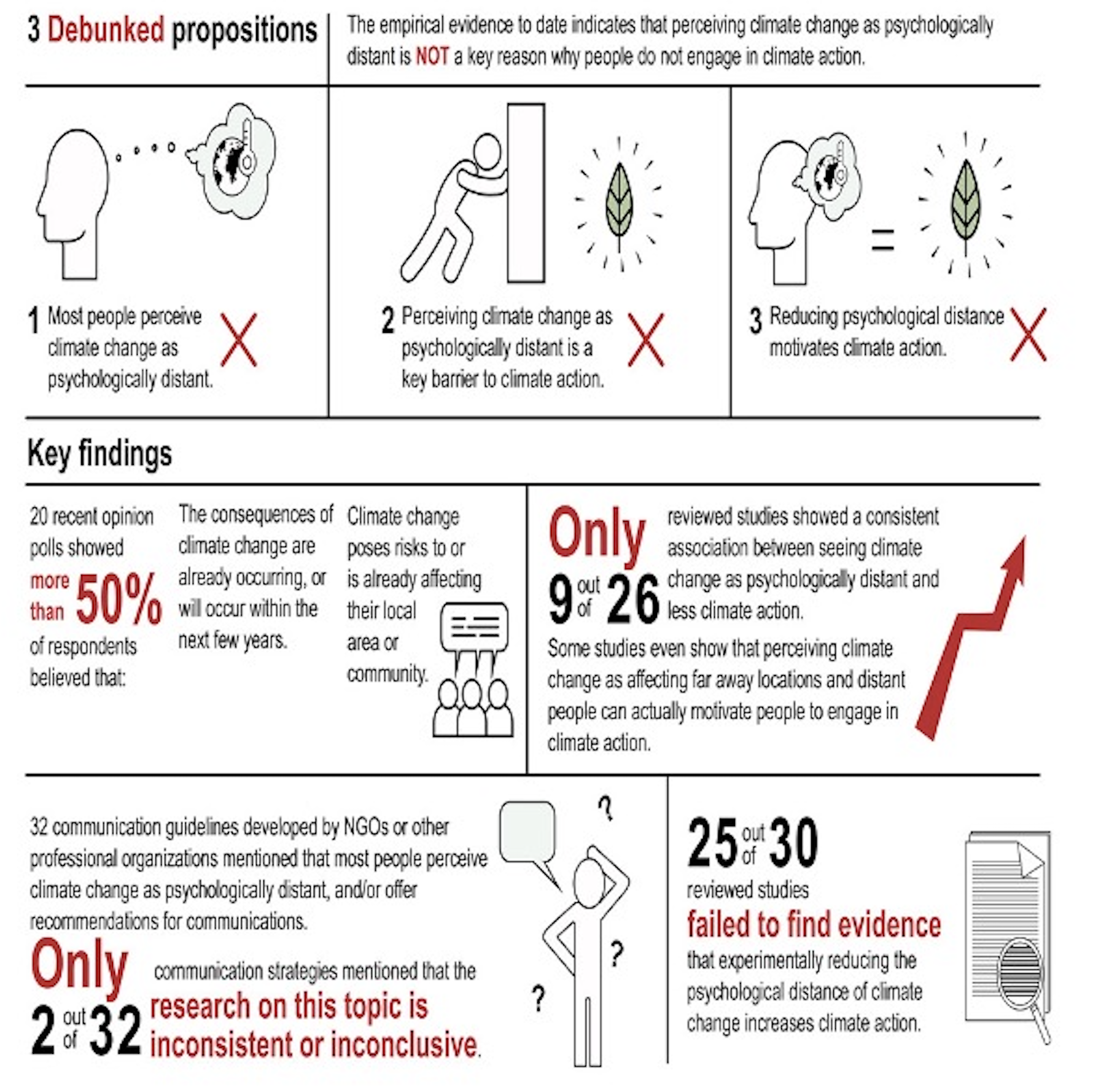
Valkengoed, Steg, & Perlaviciute, 2024, Cell.Com (8)
In partnership with groups such as the Planning and Conservation League of California, 350.org, and the International Transformational Resilience Coalition, there is hope for larger scale training models that supports the well-being of climate scientists and advocates, as well as cities and countries in their approach to navigating the intersection of climate change with societal structure. There is no suggestion that I/we do or even can know the full answers. As progressive thinker Nora Bateson writes, “the problems we are facing are so complex it is not possible to know how to fix them”. And we can aim for improving how we align with preventative efforts that may one day reach a critical mass for sustainable healing and change that guides the futures of all of life, not just us humans who have “specialized” ourselves as above the ecosystem that sustains us.
To hear a bit more about these efforts, where my interacting roles in physiotherapy, mental health, and public health merge, you can watch the below presentation/discussion that looks at climate change, disaster response, and community preparedness. I welcome your critical inputs, so that I may continue to learn and deepen into epistemic and cultural humility. I believe it is only from that stance that we will be successful and learning and growing together in interdependence with the earth and all the relatives within and upon it.
References
Header image by Markus Spiske on Unsplash
- Justice C, Sullivan MB, Van Demark CB, Davis CM, Erb M. Guiding Principles for the Practice of Integrative Physical Therapy. Physical Therapy. 2023 Oct 10;pzad138.
- Maric F, Chance-Larsen K, Chevan J, Jameson S, Nicholls D, Opsommer E, et al. A progress report on planetary health, environmental and sustainability education in physiotherapy – Editorial. European Journal of Physiotherapy. 2021 Jul 4;23(4):201–2.
- https://environmentalphysio.com/
- https://www.ioptmh.org/
- https://criticalphysio.net/
- Nicholls, David A., Birgitte Ahlsen, Wenche Bjorbækmo, Tone Dahl-Michelsen, Heidi Höppner, Anna Ilona Rajala, Robert Richter, et al. “Critical Physiotherapy: A Ten-Year Retrospective.” Physiotherapy Theory and Practice, n.d., 1–13.
- https://cmbm.org/impact/research/
- van Valkengoed AM, Steg L, Perlaviciute G. The psychological distance of climate change is overestimated. One Earth. 2023 Apr 21;6(4):362–91.