I remain unsure how to start this blogpost. The only thing that seems fairly clear is that I am trying to make sense of the current COVID-19 pandemic and I suspect that the same is true for many others. Because of my recent preoccupation with the implicit and explicit relationship between healthcare, physiotherapy and all things environment, it’s maybe not so surprising that I’ve been wondering if and how any of what we are going through with COVID-19 at the moment has anything to do with ‘environment and physiotherapy’. To be clear, I am as far from being an expert in what is currently going on as many of us, so I’m likely getting things wrong and things will continue to change as we learn more (not to mention that my choice of references here might not be ideal all the way through). So what you will read here is as a snippet and stepping stone in my sense-making and I’m more than happy to learn that I am wrong. But as the days progress it seems that my general intuition is on the right track. Simply put, this has EVERYTHING to do with the environment. Let me try and think through at least some of the ways in which this is the case.
Human-animal-environment relations
To start from what seems like some kind of beginning, COVID-19 is a zoonotic disease, a disease that can be transmitted between animals and humans and it is estimated that ¾ of all new or emerging human diseases are transmitted from animals (see CDC info on Zoonotic Diseases | One Health). If you look at some of the graphics in this visual history of pandemics by the World Economic Forum (WEF), you will see that some kind of animal to human transitions has also very much been involved in most of the major deadly pandemics in the past.
So even without going any further than this, you can see how our current situation has everything to do with what I would broadly define as human-animal relations. This is a critical point. I have already tried to indicate this in two blogposts before (here and here), but I think that thinking about and acting upon human-animal relations is categorically indispensable to a forward-thinking approach to healthcare. So this affords me with yet another opportunity to clarify what I was thinking of when I started thinking about the possibility of an environmental physiotherapy: This is not just about climate change, or about using less plastics and similar in clinical practice. It is certainly also about those things, but it is also much more and human-animal relations is most definitely also part of it. They are heavily undertheorised in physiotherapy and this is clearly no longer a tenable situation.
Moving on, it is not yet entirely confirmed what animal COVID-19 was transmitted from though assumptions are that it was passed on from faeces droppings from Bats to Pangolins as these snuffle through leaves in their search for insect, and from there to other mammals/pangolins, and then to humans (also mammals, just to be clear). This assumption is largely based on the finding that there is a 99% percent match between human and pangolin COVID-19 DNA). If you like squeezing a video in with your reading about all this, I recommend this one on the Origins of the New Coronavirus.
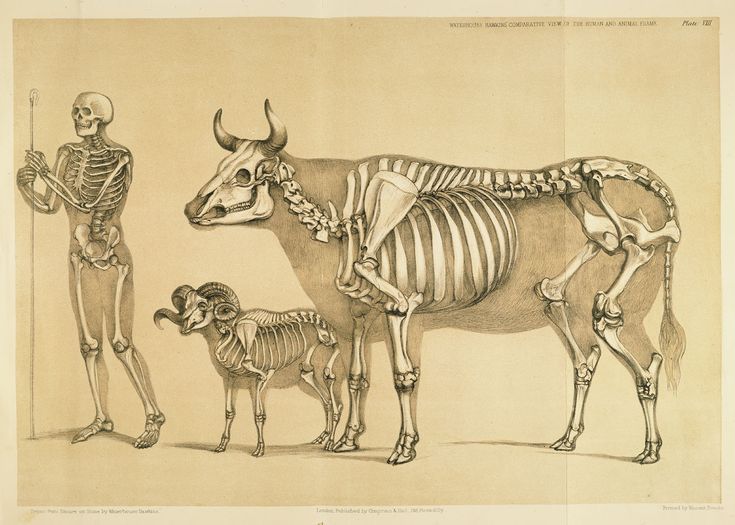
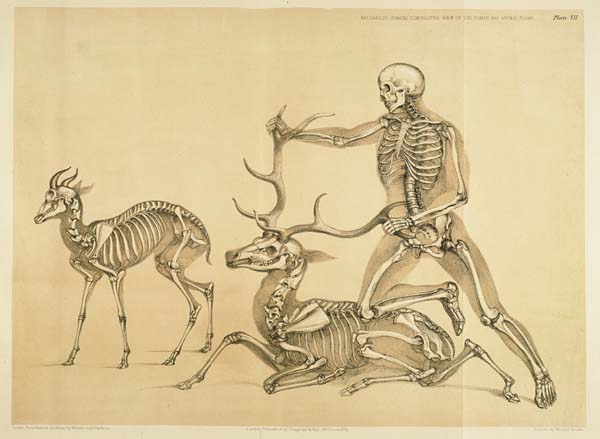
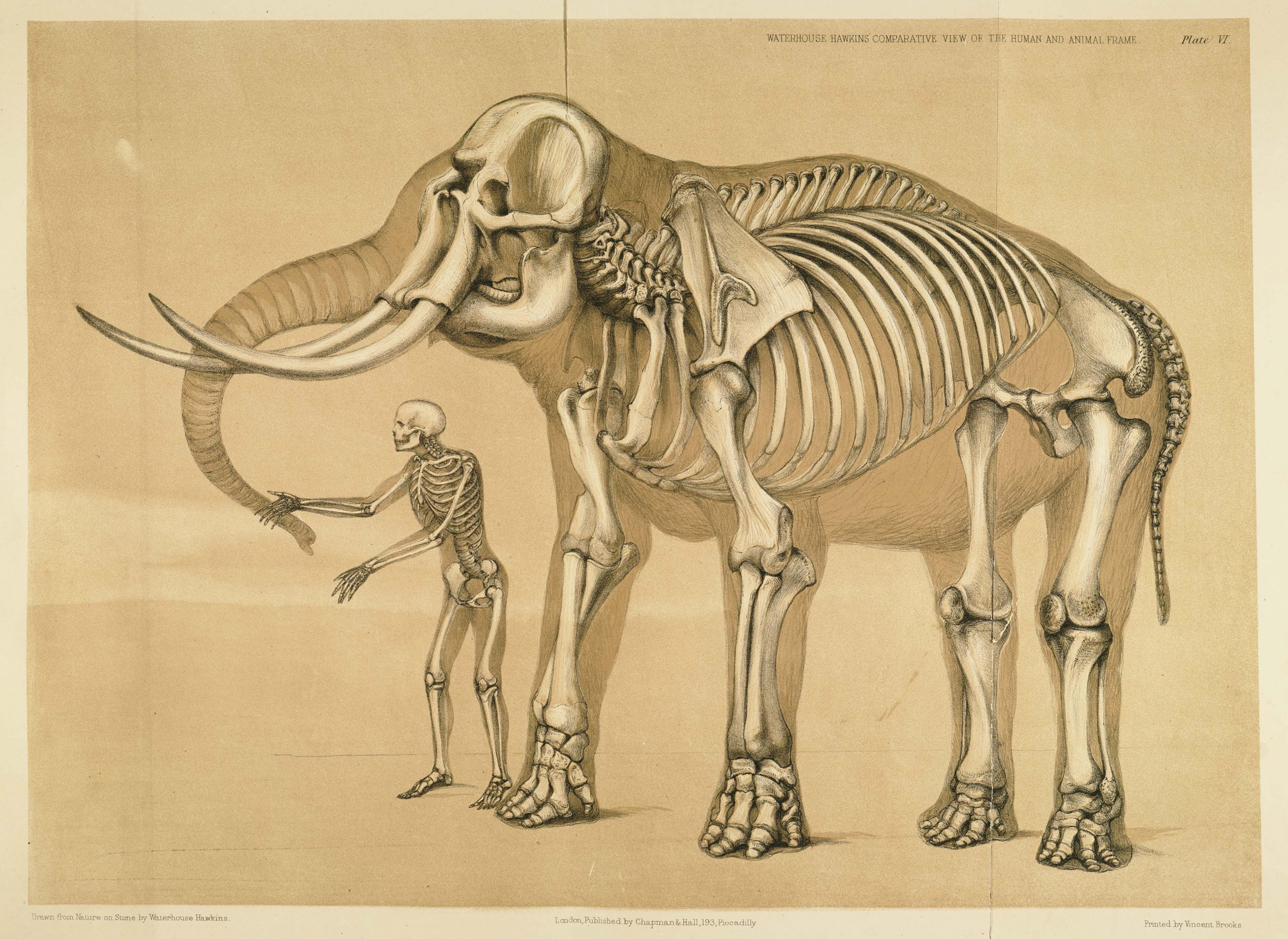
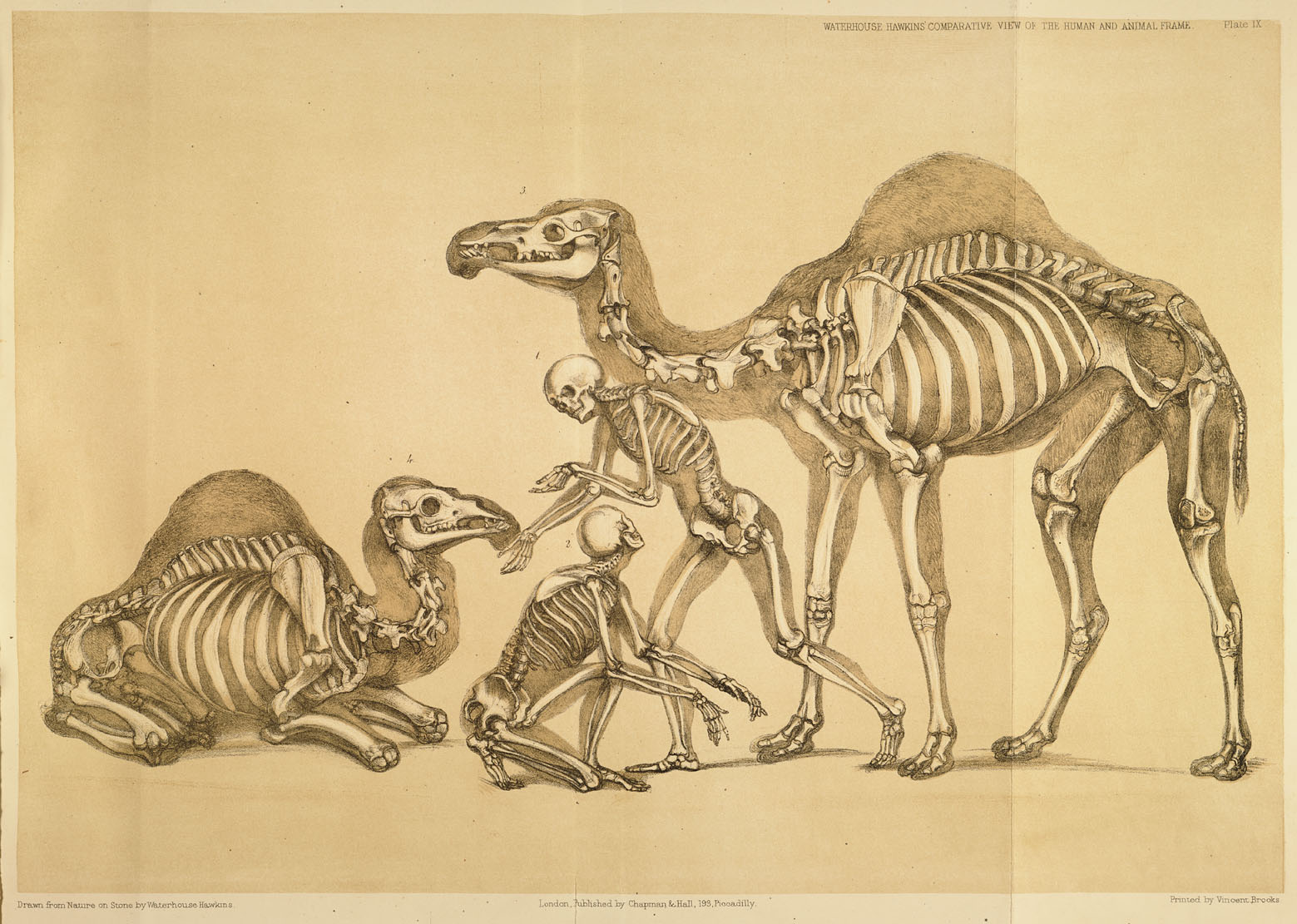
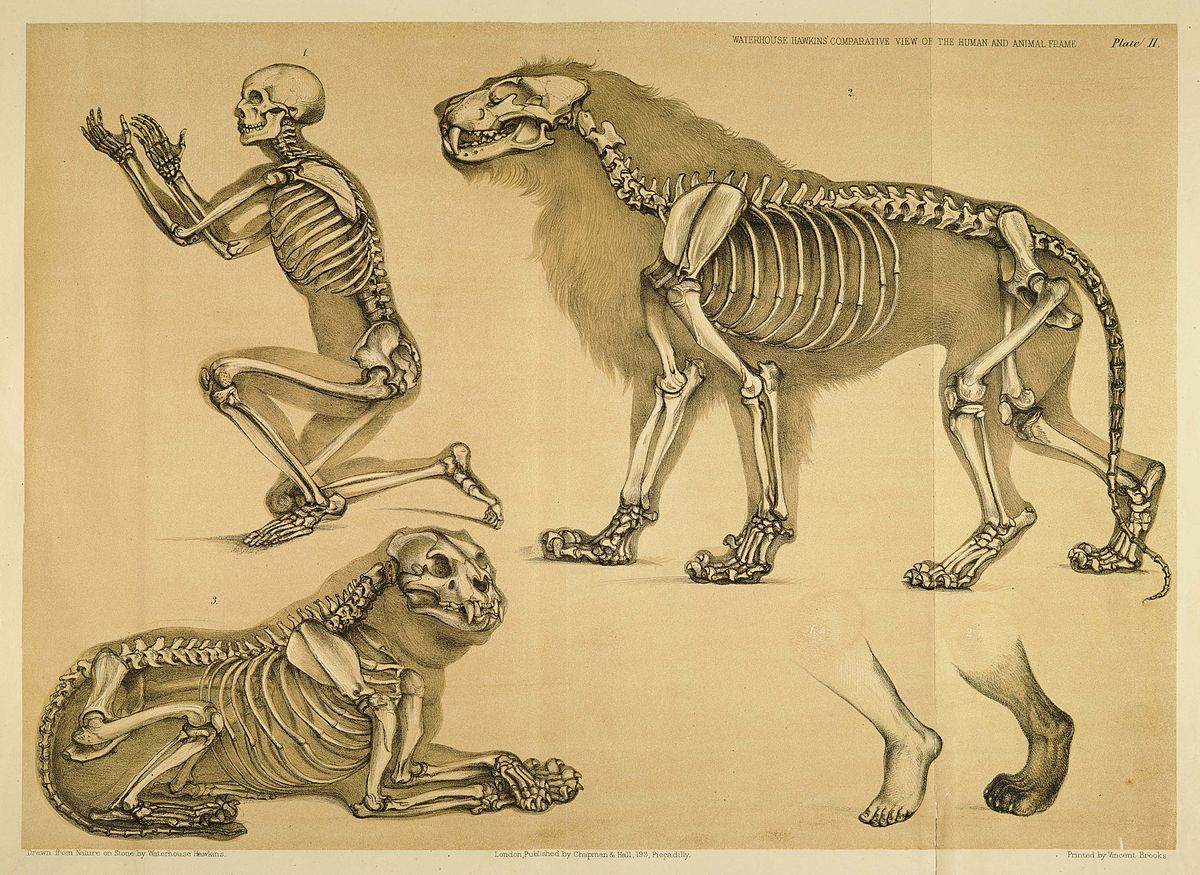
The images I have chosen to use in this blogpost come from a book by Benjamin W. Hawkins titled A comparative view of the human and animal frame published in 1860. When I came across them they immediately struck me as incredibly fitting. As a biomedically trained physiotherapist, I am immediately drawn to them. I see bones. I see similarities. Oh fun. I want to treat. I want to move joints. But look more closely, and I’ve only chosen a few examples from the book and you will see a range of human-animal relations depicted and this is where I think the meat is (excuse the pun.. the meat being invisible.. bones.. you know). The ones that irk me the most are also the most frequent ones in the book. They are the ones that depict a kind of master-slave relation where the human dominates and towers over the animal that is either in human service or the human’s victim. This kind of relationship is one of the key problems in human-animal relations around the world and it is such a huge contributor to our current predicament (and past and present like events).
There would be far less of a problem with bats, pangolins, civets, and other wild animals potential to transmit diseases if we left them in the wild. But we don’t. Wildlife hunting, farming, and trade are rampant around the world (not just in China) as we use them for our own entertainment as exotic pets, as luxury foods, status symbols, for false medicinals, and to be fair, in some cases also for mere sustenance. And in the process of all this, we drive species after species to extinction in a time when all sorts of other human driven process have brought us into the middle of Earth’s sixth mass extinction.
This is not just about our relationships to animals by the way. It is about our relationship to the environment in general, and really, these two are ultimately inseparable. As human populations grow, we continue to destroy and encroach on vital animal habitat, bringing us into closer proximity and viruses they may carry. Extractive environmental degradation and devastation, habitat loss, biodiversity loss, air travel, greenhouse gas emissions, and so many more environmental issues and the spread of infectious disease all go hand-in-hand.
‘Disease and illnesses have plagued humanity since the earliest days, our mortal flaw. However, it was not until the marked shift to agrarian communities that the scale and spread of these diseases increased dramatically. Widespread trade created new opportunities for human and animal interactions that sped up such epidemics. The more civilised humans became – with larger cities, more exotic trade routes, and increased contact with different populations of people, animals, and ecosystems – the more likely pandemics would occur. Urbanisation in the developing world is bringing more and more rural residents into denser neighbourhoods, while population increases are putting greater pressure on the environment. At the same time, passenger air traffic nearly doubled in the past decade. These macro trends are having a profound impact on the spread of infectious disease’ (WEF, 2020).
To give one more example and finish of this basic train of thought about the human-environment relations being fundamental to our current situation, I find another point really interesting. From what I understand, it is fairly certain that the majority of COVID-19 transmission happens through droplets. But isn’t it somehow uncanny that COVID-19 not only clings on to surfaces, but clings on precisely to those surfaces the longest that are already so deeply implicated in our environmental crises and associated health impacts, namely, steel and plastic. Our unwholesome relationship to nature comes to haunt us from every angle as the effects on our own health and that of other species double up.

Filip Maric (PhD)
PT, EPA Founder
Filip Maric is a physiotherapist and researcher interested in the outer rims of healthcare and physiotherapy, practical philosophy, ethics, #EnviroPT, planetary health and sea kayaking.
#SpatialDistancing and #SocialConnection
The next thing that I found interesting and that to me so obviously screams environmental issue is this whole issue around quarantine. Thankfully the psychological impact of quarantine and how to reduce it has been picked up relatively quickly. I’ve also seen that people are gradually moving away from the worrisome Social Distancing term and towards others, and following inspiration from a friend of mine, I’m still most comfortable with promoting #SpatialDistancing AND #SocialConnection.
Add to this the now increasingly confirmed, positive effects of green and blue space exposure on mental health and the picture because more complex still. Or maybe the other way round, it worries me to think what the prolonged deprivation from green and blue space exposure does to our health? Though flying under the radar, it is something that is already so gravely rampant for other reasons, it worries me to think how it might be exacerbated in our current situation.
Social/environmental determinants of health
The even bigger point about the quarantine issue, however, is the way in which it so clearly points to the socio-economic gradient and the social determinants of health. There are so many aspects to this, I can barely touch on a few.
The majority of people around the world do not have the opportunity to isolate from others as they live in environments where you can neither separate from others, nor necessarily have access to health and wellbeing supportive green and blue spaces. Many low-income families, as well imprisoned people (often overlapping populations), are more likely to live in smaller quarters and share bathrooms and kitchens with multiple people and they are often also deprived of natural environments that lend themselves to outdoor recreation (some good reading here). So to have either of these is a privilege. If you are in a situation like me, where you can isolate and have direct access to a forest and coastline on which you can keep good distance from others, you, like me, are lucky. It’s just not the case for most.
And just to reiterate, living in poor socio-economic circumstances, or areas, and living in or close to areas with heavy environmental devastation are often overlapping. And shamefully, this is often not by chance as you will quickly find as you read about environmental justice and environmental racism.
Air pollution and greenhouse gas emissions
The relationship between COVID-19 and air pollution is another interesting example for this and lends itself to adding still more complexity. ‘Globally, outdoor air pollution caused three million premature deaths in 2012 – roughly the same as the toll from malaria, tuberculosis and HIV/AIDS combined. Pollution affected health and quality of life throughout the life course, with evidence of links to cancer, asthma, stroke, heart disease, diabetes, obesity, changes linked to dementia, and harmful effects on the foetus and young child’ (quote from here). As air pollution is a major problem in, for example, India, and COVID-19 has been proven to affect those with prior lung infection more severely, doctors are arguing that people living in regions with high levels of air pollution and, consequently, already compromised lung function are more vulnerable to the spread and consequences of COVID-19. Some of this is yet to be proven, though I think it should be fairly easy to see that there is some high likelihood here. If you additionally consider that poor people suffer exponentially more from air pollution, also due to the polluted conditions they live in, well, you can do the math.
So what adds complexity, or maybe a rather ironic sliver of hope is evidence that greenhouse gas emissions, specifically, airborne nitrogen dioxide has plummeted over China due to economic slowdown and transportation shutdown associated with the COVID-19 outbreak. More news along these lines now seem to be coming in by the day (see here). So it’s rightly been suggested (here) that the current pandemic might be showing us either what things might be like if we don’t improve our relationship to the environment and pandemics, air pollution, etc. become ever more frequent and widespread or, conversely, show us that we can indeed act resolutely and with significant positive impact if we believe it sufficiently important and urgent.
Wet markets, digital health and digital education
So this gradually moves our thinking toward the question what we can do and I personally think there are many many different opportunities. What seems to be getting the most attention at the moment, at least in my little world, are digital health and digital education. I have to admit though, as much as I am grateful for the possibilities digital life provides, which are likely specifically in the area of #SocialConnection and working from home, I am also worried about what all this might mean and lead to. This partially latches on to the issues around quarantine, but let me try think through this via a range of questions that keep circling in my head:
Do people also need, not just social, but as a critical part of this, also physical contact to other people and their natural environments? Do they maybe often need more than they currently have in their daily lives? Is increasing digital health and education capacities the right way to go then, when we must actually do everything we can to reduce the need for digital health resulting from situations like these?
As people are aggressively arguing for health insurers to pay for telehealth, and possibly for it being equally as effective, will this lead to insurances recognising the economic potential of not paying for face to face treatments anymore? Will we then have to reverse argue the importance of face to face treatments again? Will the same happen for universities, which are now all switching to digital education? Is the consequence of this even less physical contact with other humans and even less physical contact with and exposure to natural environments as people spend more time yet again in front of their screens?
More to environmental issues, where is the evidence that an aggressive switch to more digital health and education is actually more environmentally friendly? Are we pretending as though this is not made possible by increased needs for and use of energy and natural resources? Where does this energy come from? What about the natural resources (rare minerals, etc etc) that are required to build the devices that we communicate, teach, and treat on, or get treatments and education through? Are this energy and these resources not generated through further environmental and social devastation? Does, then, our celebration of digital health and digital education not provide still more evidence in our belief in technofixes to our current social and environmental crises? Does it not deter us from looking in the directions that actually need fixing?
I could not be further away from having the answers to all of the above questions, though I am certain that my bias is relatively visible in them. The key point maybe is that solutions are never as simple, or as unproblematically good as we would like them to be. In relation to digital health and education, this must very much relate to recognising that their difficulties do not just lie in finding out how to deliver ‘good’ digital health or education. That already assumes too much about the goodness of them in a kind of general, abstracted manner that precisely does not ask questions like the above.
We could also take the example of wet markets to reiterate how difficult it is to find solutions. Wet markets are where live wild animals are sold, and where they consequently also discharge (urine, faeces, mucus, and potentially also blood, though this is not discharged as much as a result of injury or being slaughtered), which then in turn also enables the transmission of zoonotic diseases. The simple intuition would be to think that we just have to undo with them and in some cases this might also be true. As this recent Guardian article nicely argued however, it often also isn’t true because vast amounts of people depend on these markets for their food, sustenance and financial survival. In fact, some of the people that need these wet markets live in the same minerals that we need for our digital health and education continue to be mined and continue to be socially and environmentally devastated for ‘our’ health and education.

Reinventing healthcare
Clearly the first thing to do then is not to be naive about our problems and the solutions we come up with in their wake. I am inevitably going to talk myself into a corner here, because the same must apply to whatever ‘things to do’ I suggest here, but what can you do. I do know that we are all trying our best and so am I, biases and all.
The next thing to do, as physiotherapists, is to truly take to heart what Dr Mike Landry argued in his recent interview on the Global Physio Podcast:
“Let’s not think about physio anymore as being about NCDs, let’s just think of ourselves as participants in healthcare. Full stop.”
To put this in other terms that I have and continue to argue via the idea of environmental physiotherapy, we must start looking at and acting on a far bigger picture still. The threat for more pandemics is rising as social and environmental devastation rage rampant around the world. So if we really want to do something to prevent future pandemics like the current one, and not just be more and more skilled in fire fighting, we must understand and act on the bigger picture. In extension to what has been noted in relation to the issues around air pollution (which go hand in hand with poverty, caste, and more) ‘the only way… to fight COVID-19 or future pandemics would be if the environment is protected’ and I will add, if we address some of the related social issues. This kind of bigger picture healthcare is precisely what is argued across planetary health, sustainable healthcare and the likes. And if the current situation is making anything clear, it is that we must make them central to our thinking.
I have to admit that, at least for me, personally, this also means letting go of the idea that we are some kind of ‘movement specialists’. I am struggling not to go down this rabbit hole as I am writing (to self: don’t do it Filip), but I really have a problem with this conception and many arguments against it have already been made over the years. Sadly, with relatively little effect. In short, I doubt that we are movement specialists. We still don’t even have a clear conception of what we are talking about when talking about movement, and we clearly no only very little about the movement of infectious disease, to take just one example. And this is not to mention that I think there are many people out there, professional and non-professional that can contest with our claim for specialisation, easily. I believe that we are and must be something else, though I am aware that this needs much further (or continuous) thought and refinement.
“Let’s not think about physio anymore as being about NCDs, let’s just think of ourselves as participants in healthcare. Full stop.” Dr Mike Landry on the Global Physio Podcast.
So to move away from such pigeonholing and to a very few examples, I believe we could and should likely get involved in advocating and advancing plant-based diets and food production, alongside any other planetary health practitioner. We must also advocate and advance social and environmental awareness and responsibility, in healthcare and beyond. We must support ‘movement’ away from (wild) animal trade, farming, and just simply, abuse. We must educate people about harmful beliefs in the medicinal potential of animal parts and particular slaughtering methods. We must advocate and advance appropriate housing for everyone, human, plant, animal, or else. We must study other modes and avenues of thinking to open up our minds to new ways forward. The list goes on.
It is argued that our current situation is more than just an enormous cluster of crises, but also a historic opportunity to reinvent our economies towards more environmentally aware and responsible solutions. What I would add to that then, is that it is also a historic opportunity to reinvent healthcare systems and provision along the same lines (and of course the two go hand in hand).
It’s amazing to witness people whizzing together all these online courses and handbooks at the moment and these efforts can only be applauded. But if we are going to teach about infectious, or any other diseases in physiotherapy or health, maybe this is the greatest opportunity to start from the environmental and social issues that are driving the increase and faster and easier spread of infectious diseases, NCDs, malnutrition, trauma, injury, etc. Let’s go to the causes, rather than just fight the symptoms – a concept that we understand very well. Let’s go to our relationships to other humans, animals, plants, you name it.
I really hope that this nightmare will pass very soon and without much further suffering. I am as frightened and terrified as anyone. Yet to me all this also clearly points to the fact that there is just ever more reason and, in fact, urgency, to develop and advance a healthcare that respects humans, animals, and all of our shared environment on this planet, and builds on the inseparable relationship between us all. Call it planetary health, call it environmental physiotherapy. Whatever you prefer and whatever works best in your context. But as we have recently very stated in the EPT Agenda 2023, I’m going to stick my neck out here and repeat it, I have a strong sense that the time to reinvent healthcare in this manner is now.
Be well, healthy, and safe, and above all else, let’s always be kind to each other. I hope I have managed to keep this post in the same spirit.
Filip
Post Scriptum
In the meantime a whole host of new blogposts, articles and videos on the broader topic of this blogpost have been published, including some additional points that I did not cover or only briefly pointed to. I will continue archiving some of the particularly good resources here as I continue coming across them in the hope that they will eventually inform a much deeper discussion about environmental awareness and responsibility in physiotherapy:
1) Inayatullah, S., & Black, P. (2020_03_18). Neither a Black Swan nor a Zombie Apocalypse: The Futures of a World with the COVID-19 Coronavirus. Journal of Futures Studies (jfsdigital.org).
2) van Dooren, T. (2020_03_22). Pangolins and Pandemics: The real source of this crisis is human, not animal. New Matilda (newmatilda.com).
3) Morton, T. (2020_03_ 23). COVID-19 Ecological Cultural Criticism class series:
Class 2 – Eco awareness and our sense of words; What would ecological awareness do to our deep deep sense of what words like “see” and “idea” mean? Incl. some good utopian things to hold on to.
Class 3 – Ecofascism and the human as virus; including thoughts on racism and the uncanny valley, abjection and patriarchal logic, and toilet paper.
Class 4 – Beauty is a virus, beauty is death, sexual display implies the infinite spectrum of sexualities, sexual selection is as non-teleological as natural selection and symbiosis
Class 5 – Sexual selection is driven by females and has nothing to do with wealth, power or utility, and everything to do with beauty as the phenomenology of coexistence
Class 6 – tbd
4) Carrington, D. (2020_03_25). Coronavirus: ‘Nature is sending us a message’ says UN environment chief. The Guardian.
5) Lowe, C. (2014). Infection. Environmental Humanities, 5 (1): 301–305. doi: 10.1215/22011919-3615559
6) Kock, R.L., et al. (2020). 2019-nCoV in context: lessons learned? Lancet Planetary Health, 4(3): PE87-E88. doi:10.1016/S2542-5196(20)30035-8
7) Morley, R. (2020). A tale of two emergencies. Lancet Planetary Health, 4(3): PE86. doi:10.1016/S2542-5196(20)30062-0
8) Porter, N. (2012). Risky Zoographies: The Limits of Place in Avian Flu Management. Environmental Humanities, 1(1): 103–121. doi:10.1215/22011919-3609994
9) The Club of Rome (2020_03_26). Open Letter to Global Leaders – A healthy planet for healthy people. Call to Action from the Planetary Emergency Partnership: Emerging from the Planetary Emergency and partnering between People and Nature (clubofrome.org)
10) Carrington, D. (2020_03_24). Coronavirus poses lethal threat to great apes, experts warn. The Guardian.
11) Gillespie, T.R., Leendertz, F.H. (2020_03_24). COVID-19: Protect great apes during human pandemics. Nature: 579, 497. doi: 10.1038/d41586-020-00859-y
12) Figueres, C. (2020_03_24). 5 Lessons from Coronavirus that will help us tackle climate change. Time Magazine.
13) Beitsch, R. (2020_03_26). EPA suspends enforcement of environmental laws amid coronavirus. The Hill.
14) Miller, R. (2020_03_26). Foresight in a Time of Coronavirus – Riel Miller (Head of UNESCO Futures Literacy). Episode 41. Future Pod.
15) Ervin, J. (2020_03_27). Applying the hard lessons of coronavirus to the biodiversity crisis. UN Development Programme.
16) Andreas Chatzidakis, Jamie Hakim, Jo Littler, Catherine Rottenberg, & Lynne Segal (2020_03_26). COVID-19 pandemic: A crisis of care. The Care Collective. Verso (Blogpost).
17) Stein, Z. (2020). COVID-19: A war broke out in heaven. Emerge / What is emerging?.
18) Canby, K. (2020_27). Ending illegal deforestation is good for our health (commentary). Mongabay.
19) Lynteris, C., & Fearnley, L. (2020_03_02). Why shutting down Chinese ‘wet markets’ could be a terrible mistake. The Conversation.
20) FILAC (2020_26). Our Declaration on the COVID-19 pandemic from the Board of Directors to Member States (of the UN). Fund for the Development of Indigenous Peoples of Latin America and the Caribbean. La Paz, 26 March 2020.
21) Nicholls, D. (2020_03_30). Physiotherapy in a time of pandemic. International Physiotherapy History Association (blogpost).
22) Nicholls, D. (2020_04_01). Physiotherapy in a time of pandemic – an addendum. Critical Physiotherapy Network (blogpost).
23) Keck, F. (2020). Avian Reservoirs: Virus Hunters and Birdwatchers in Chinese Sentinel Posts. Duke University Press; Durham, USA.
24) Armstrong, F., Capon, A., McFarlane, R. (2020_03_30). Coronavirus is a wake-up call: our war with the environment is leading to pandemics. The Conversation.
25) Nasi, R., Fa, J.E. (2020_03_30). COVID-19-led ban on wild meat could take protein off the table for millions of forest dwellers. Forests News. DGs Column.
26) Andersen, K.G., Rambaut, A., Lipkin, W.I., Holmes, E.C., Garry, R.F. (2020_03_17). The proximal origin of SARS-CoV-2. Nature Medicine. doi:10.1038/s41591-020-0820-9
27) Thomas, P., et al. (2020_03_30). Physiotherapy management for COVID-19 in the acute hospital setting: clinical practice recommendations. Journal of Physiotherapy. In press, journal pre-proof. doi:10.1016/j.jphys.2020.03.011
28) Haines, K.J., & Berney, S. (2020_04_02). Physiotherapists during COVID-19: usual business, in unusual times. Journal of Physiotherapy. In Press, Journal Pre-proof. doi:10.1016/j.jphys.2020.03.012
29) Collyns, D., Cowie, S., Parkin Daniels, J., Phillips, T. (2020_03_30). ‘Coronavirus could wipe us out1: indigenous South Americans blockade villages. The Guardian.
30) Watts, J. (2020_04_03). Brazil: Coronavirus fears weaken Amazon protection ahead of fire season. The Guardian.
31) Carusi, A., & Schillace, B. (2020_03_27). Coronavirus – bodies, environments and the spread of disease. BMJ Talk Medicine (podcast).
32) McCartney, M. (2020_03_31). Medicine: before COVID-19, and after. The Lancet, online first. doi:10.1016/S0140-6736(20)30756-X
33) Foley, J. (2020_04_03). After the Storm. Global Eco Guy, The Medium.
34) Morton, T. (2020_04_04). Thank Virus for Symbiosis. STRP Festival 2020 – The Corona Essays.
35) Daly, N. (2020_04_05). Tiger tests positive for coronavirus at Bronx Zoo, first known case in the world. National Geographic.
36) Andersen, I. (2020_04_06). UNEP Statement on COVID-19. UN Environment Programme.
37) Wei-Haas, M. (2020_03_31). Key ingredient in coronavirus tests comes from Yellowstone lakes. National Geographic.
38) Sarasin, P. (2020_03_25). Mit Foucault die Pandemie verstehen. Geschichte der Gegenwart (blogpost).
39) Robinson, D. (2020_04_03). Coronaviruses: are they here to stay? UN Environment Programme.
40) Hartigan, J. (2020_04_07). Social Distancing: A Multispecies Perspective. Society for Cultural Anthropology (blogpost).
41) Wu, X., Nethery, R.C., Sabath, B., Braun, D., Dominici, F. (2020_04_05). Exposure to air pollution and COVID-19 mortality in the United States. A national study on long-term exposure to air pollution and COVID-19 mortality in the United States. Harvard University.
42) Boffey, D. (2020_04_08). Amsterdam to embrace ‘doughnut’ model to mend post-coronavirus economy. The Guardian.
43) Raworth, K. (2020_04_08). Introducing the Amsterdam City Doughnut. Kate Raworth: Exploring Doughnut Economics (blogpost).
44) Timothy, R.K. (2020_04_06). Coronavirus is not the ‘great equalizer’ – race matters. The Conversation.
45) Steinberger, J. (2020_04_08). Pandenomics: a story of life versus growth. Open Democracy (blogpost).
46) Roe, D. (2020_04_01). Despite COVID-19, using wild species may still be the best way to save them. International Institute for Environment and Development (blogpost).
47) Kappelle, M. (2020_04_08). Six nature facts related to coronaviruses. UN Environment Programme.
48) Vaughan-Lee, E. (2020_04). Shaking the Viral Tree: An Interview with David Quammen. Emergence Magazine (Podcast).
49) Akomolafe, B. (2020_04_16). I, Coronavirus. Mother. Monster. Activist. Emergence Network (Essay).
50) Smith, W., & Theriault, N. (2020_04_16). Seeing Indigenous Land Struggles in the “Multispecies Cloud” of Covid-19. Society for Cultural Anthropology (blogpost).
51) Miller, R. (2020_03_28). Out of the Ashes.
52) Maric, F. & Nicholls, D.A. (2020). Paradigm shifts are hard to come by: Looking ahead of COVID-19 with the social and environmental determinants of health and the UN SDGs. European Journal of Physiotherapy. doi:10.1080/21679169.2020.1826577
53) IPBES (2020_10) Workshop on Biodiversity and Pandemics – Workshop report. This report details that: COVID-19 is the 6th global pandemic since the Great Influenza of 1918; that pandemics are becoming more frquent, mroe costly and more deadly; almost all known pandemics and 70% of emerging diseases come from microbes carried by animals; but the emergence of pandemics is entirely driven by human activities; the same human activities that drive climate change and biodiversity loss also drive pandemic risk; these include land-use change, agricultural expansion and intensification; unsustainable trade, production and consumption; this unsustainable exploitation of the environment brings wildlife, livestock, and people into closer contact; and this is the path to pandemics; land-use change alone is responsible for more than 30% of new diseases, with 3/4 of earth’s land surface having significantly been altered by human activities; pandemic risk can be reduced by addressing many of the same drivers of biodiversity loss and climate change at an estimated cost of 100x less than the current economic impacts of pandemics; the overwhelming scientific evidence points to a positive conclusion: Prevention really is better (and cheaper) than cure!
54) Gibb, R., Franklinos, L.H.V., Redding, D.W., Jones, K.E. (2020). Ecosystem perspectives are needed to manage zoonotic risks in changing climate. BMJ, 371:m3389. doi:10.1136/bmj.m3389


I am seeing this blog post at the same time that a health equity group of which I am a member is re-posting this article:
https://www.theguardian.com/environment/2020/mar/18/tip-of-the-iceberg-is-our-destruction-of-nature-responsible-for-covid-19-aoe?CMP=Share_iOSApp_Other
I imagine that many of us are having similar thoughts.
Yes, the article is also referenced in the blogpost and it is certainly hopeful that many of us are having similar thoughts. All of this is making it ever more clear how important it is that we change our perspectives and approaches to more socially and environmentally responsible ones.